MAZE
Post Concussion Syndrome (PCS) occurs when concussion symptoms last longer than three months. On average, one out of four people with a concussion suffers from symptoms longer than 6 months, and so has PCS. There is currently no medical directive in the Netherlands for treating people with PCS. These people struggle to find the right knowledge, find the right care, and struggle with the long waiting times for care. People with PCS are lost in a maze, which causes many consequences. In this project, we will search for the roots of this problem by mapping a patient journey of PCS.
Navigating the perplexing medical landscape while suffering from PCS.
Vision
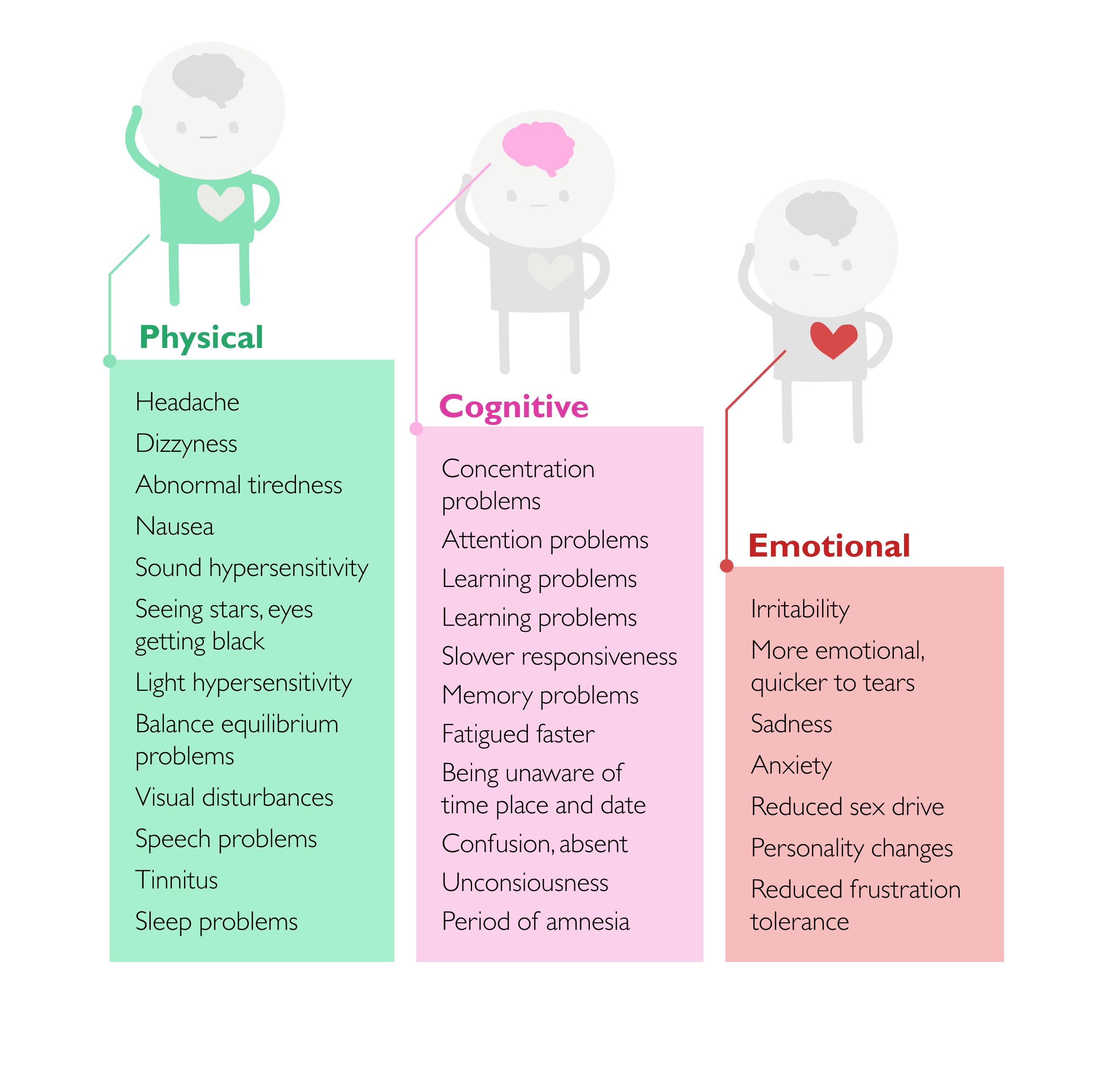
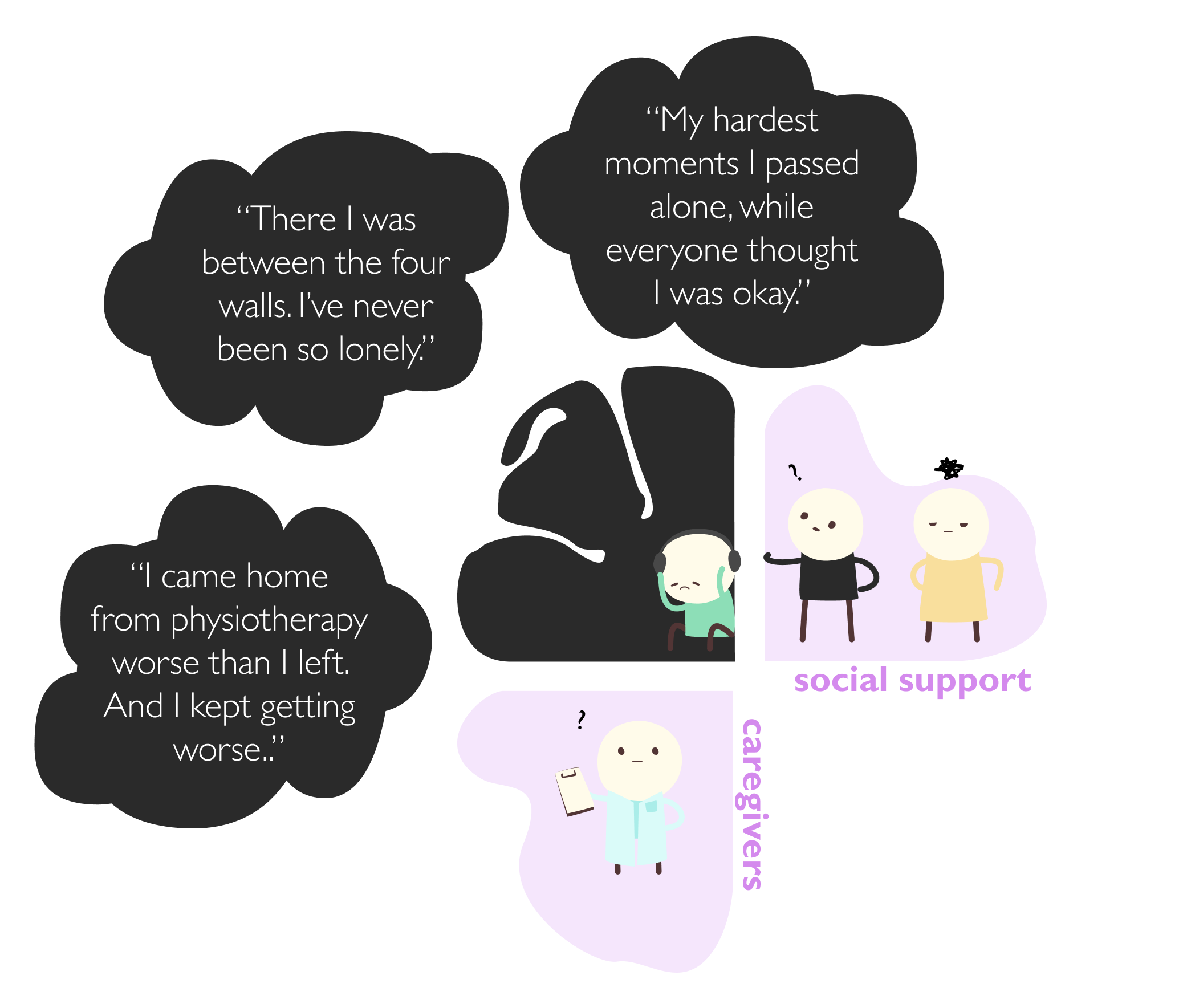
A person with PCS suffers from physical, cognitive, and emotional symptoms. Everything that entertains us makes a patient with PCS physically sick, confining them to a life of low energy and isolation. Bad days are often spent staring at walls. Social support can light up the day of people with PCS by helping them do small tasks, listening to their stories and struggles, and making them feel aware that they can depend on them. But professional help is often crucial. Since the patient often can't bear screens or process information, getting medical attention without this social support is nearly impossible. Without this, someone can feel even more lonely, miserable, and not acknowledged and recognized at all.
In many cases, the person has not even been told they have a concussion or PCS. This is caused mostly by the lack of a medical directive for the chronic phase of light brain injury and PCS. This means often GPs have no idea what they can do and what type of care they can give a referral for to a patient. Also, a patient often has to defend themselves that they are sick. Lacking a medical directive, the GP will easily think that there is no real problem and therefore not refer the patient to care. As they say, 'onbekend maakt onbemind' (unkwnown makes unloved).
Because of this lack of knowledge patients struggle to navigate their way to medical help. They are left to fend for themselves, find care on their own, and continuously defend that they are sick. This situation can make the patients feel helpless, lonely, misunderstood, unrecognized, and unacknowledged. Next to this, it leads to a lack of information on what to do and how to rehabilitate.
“Patients sometimes spend years looking for the right treatment.
This delay is detrimental to patients, …”
To solve this problem, we can try to make information accessible on websites such as thuisarts.nl, but that leaves the responsibility to the patients who already have low energy and are sick. That is why I believe the responsibility should rest with the healthcare sector and not with the patient. Our design opportunity is to raise awareness among healthcare professionals, such as NHG, about PCS and establish a medical directive for PCS.
MAZE in detail
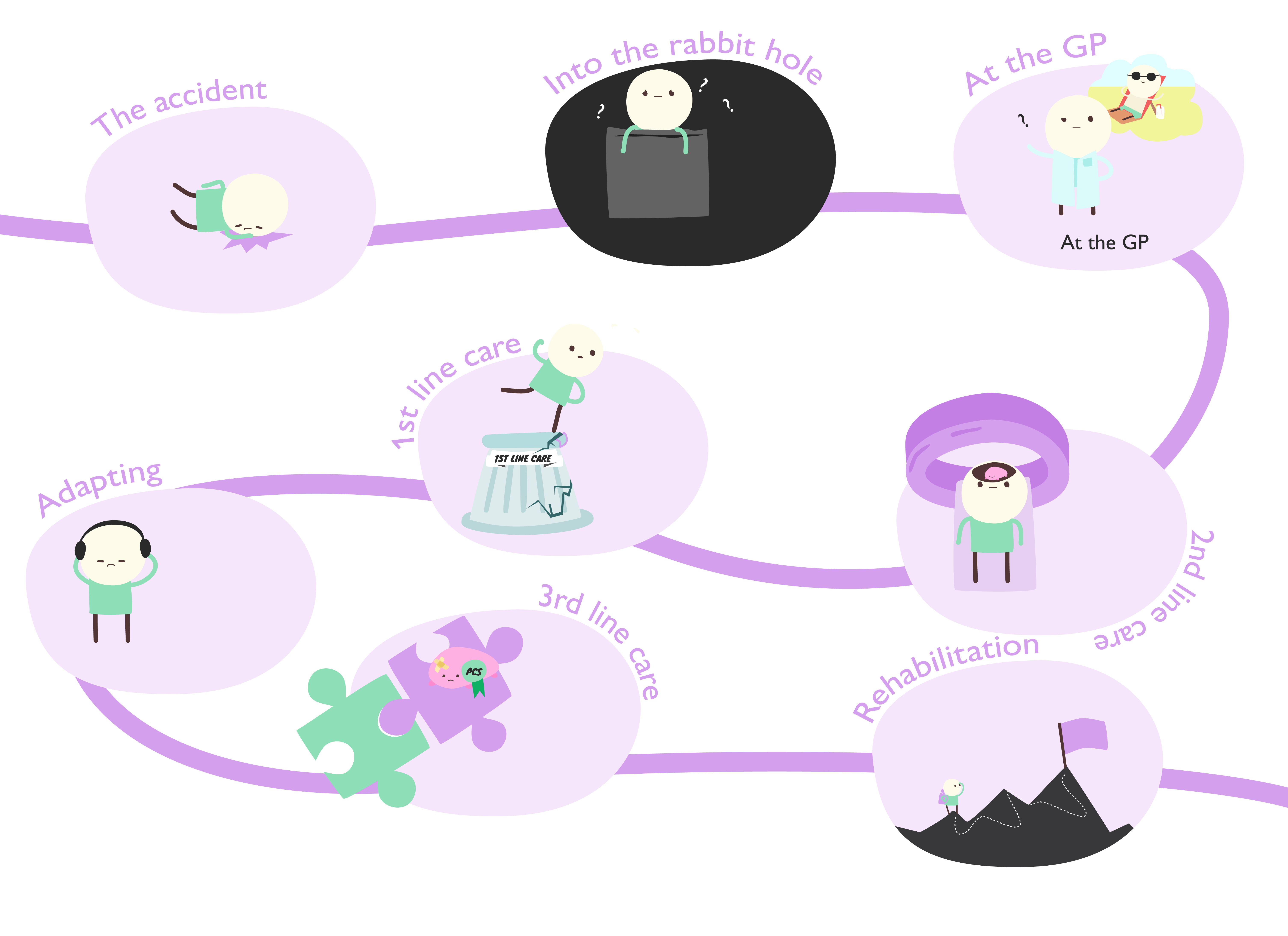
In a patient journey, the process a PCS patient goes through until he has found (helping) care has been captured. The eight phases identified are the accident (1), into the rabbit hole (2), GP appointment (3), adapting (4), 1st line care (5), 2nd line care (6), 3rd line care (7), and rehabilitation (8). For each phase, a time span, the active actors, touchpoints, the patient’s emotions, challenges, and design opportunities are thought out. With these stages, we mark the large steps the patient takes in their recovery.
The recovery starts right after the accident when the patient receives the impact against the head. When not immediately realizing the seriousness of the blow, the patient goes home with the assumption of the pain soon being over. When the pain does not go away, patients will get in contact with their GP, who will issue the following referrals, resulting in the patient slowly rehabilitating.
This is a rough description of the journey a PCS patient experiences. However, because there is no medical directive for PCS present, it can happen that patients experience some of the phases in different orders, timeframes, or not at all. Want to take a closer look at the patient journey? Click here!
MAZE the process
Together with Yulan van Es, I started on this 20 days project over the span of 10 weeks. We both are PCS experience experts and while we talked with each other about it, we found the spark that many things could be better organized in the PCS process.
We have started mapping all the active actors, based on research, blogs, and our own experiences. In this research, we already identified the lack of a medical directive, and because of this, the presence of the actors can differ for every patient.
Next, we identified the eight phases a patient generally experiences. For every phase, we identified four distinct factors. The time span shows us the duration of a phase and the incredible times that patients wait for help. The active actors and touchpoints help us identify what and who the patient encounters. The emotions allow us to reflect on what the patient goes through.
For these emotions, we analyzed blogs on patient experiences. With the help of the self-determination theory, we were able to categorize the emotions of all the different stages. For example, the quote 'I often wondered if I was going to recover and if there was any recovery at all' is a sign of feeling defeated. We identified this as a lack of perceived competence.
Based on the touchpoints and emotions we could then identify challenges from the patient's perspective. However, we found there are no medical directives on PCS, meaning we had to find out for ourselves what challenges appear on the side of the medical professionals. We, therefore, interviewed a GP, physiotherapist, neuropsychologist, and rehabilitation nurse to gain insights into the medical perspective of the problem.
Based on the created overview we were able to identify different design opportunities in every phase of the patient journey using the touchpoints, emotions, and challenges we described.
As the last step, we reflected on the whole patient journey to draw our own personal conclusions. At the end of our design research, a report from the Nederlandse Vereniging van Revalidatieartsen (VRA) spotted the same problems we found during describing our patient journey. They are currently working on a medical directive for PCS. The draft medical directive which was published after our research, adds strength to the bottlenecks we identified. This was a good check for us that we had done our research correctly.
And yay, a medical directive is on its way!
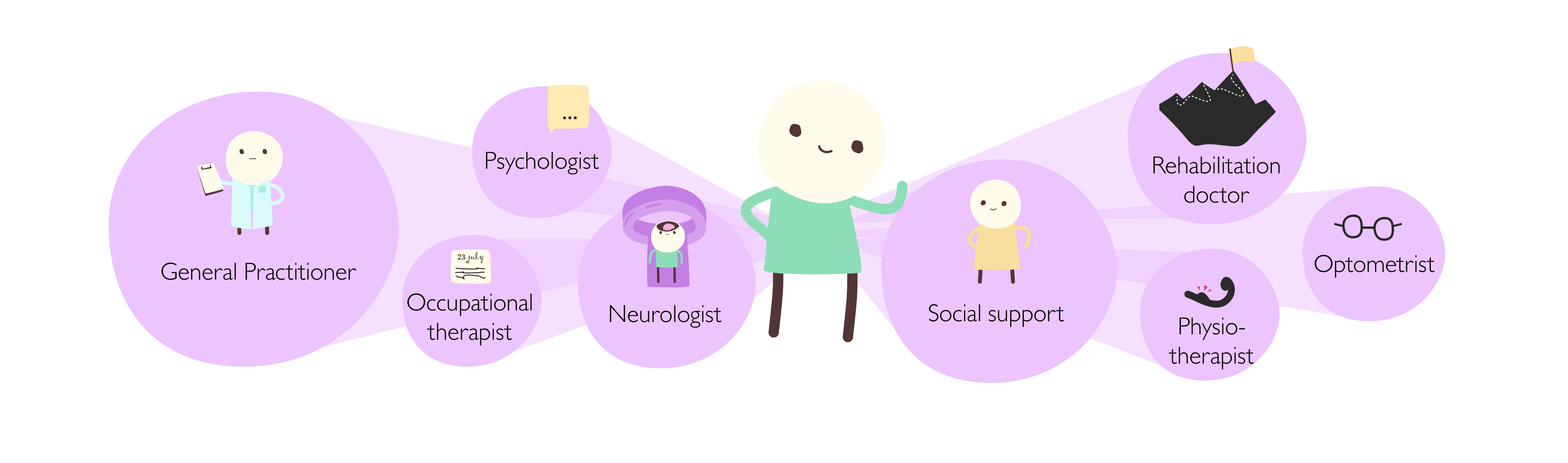
Actors
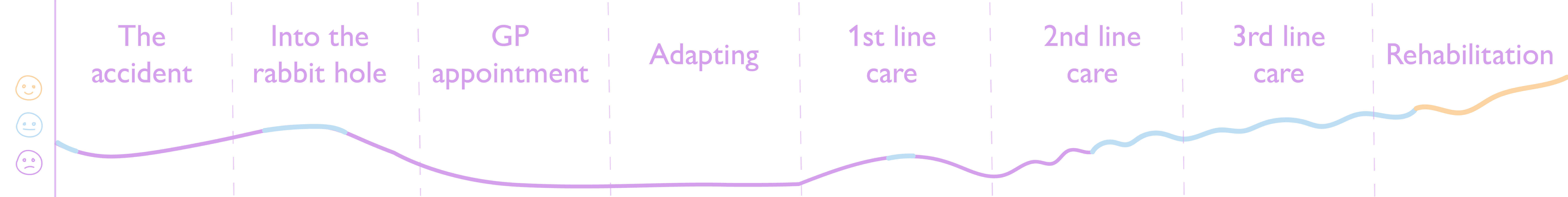
Emotions